
Age Related Macular Degeneration: What is it?
Symptoms You May Experience:
Examination: What Your Eye Doctor Will Look For:
What You Can Do:
When To Call Your M.D.:
Treatment For AMD:
Prognosis: Will I See Better?
Age related macular degeneration (AMD) is the leading cause of cental vision loss in the western world in people over the age of 55. AMD is an age-associated degenerative disorder of the macula, which is the portion of the retina responsible for central vision. In AMD the cells that make up the macula become damaged, resulting in central vision loss.
There are a number of reasons why people may develop AMD, including increasing age, genetic and hereditary factors, and environmental risk factors. Since pigment in the eyes appears to be protective, Caucasians, particularly women, appear to be at greater risk. Smoking, family history, nutrition, and sunlight exposure over the course of one's lifetime may also play a role.
There are a number of reasons why people may develop AMD, including increasing age, genetic and hereditary factors, and environmental risk factors. Since pigment in the eyes appears to be protective, Caucasians, particularly women, appear to be at greater risk. Smoking, family history, nutrition, and sunlight exposure over the course of one's lifetime may also play a role.
The vast majority of patients with dry AMD will not notice any changes in their central vision. However, patients with advanced dry AMD may notice a graduall decrease in their central vision, as well as formation of a central blind spot over many months or years. The most common symptom of wet AMD is the sudden onset of blurred or distorted central vision that may occur over days to weeks. AMD is painless.
After checking your vision and performing a routine eye exam, the eye doctor will dilate your eyes to obtain a view of the macula so that he or she can look for signs of AMD. If wet AMD is suspected, a fluorescein angiogram (photographic dye test) may be obtained. In some cases, optical coherence tomography (OCT), another photographic test, may be performed as well. The photo at left shows blood vessels and hemorrhage underneath the retina, found in the wet form of AMD.
There is currently no way to prevent AMD, although avoiding smoking and maintaining a healthy diet may help reduce the risk of developing the disease. Because AMD is a relatively silent disease untill the advanced stages develop, all patients over the age of 55 should have an annual dilated eye examination to look for early signs of AMD.
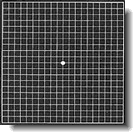
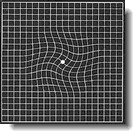
Now that treatments are available for most patients with either the dry or wet form, it is important that AMD be diagnosed as early as possible so that appropriate treatment can be started promptly. If you have AMD, regular home use of the Amsler grid (which your eye doctor may provide) can help you monitor changes in your central vision.
The photos at right show a typical Amsler grid. The top photo shows the Amsler grid as seen by those with normal vision. The bottom shows the grid as seen by someone with AMD.
Now that treatments are available for most patients with either the dry or wet form, it is important that AMD be diagnosed as early as possible so that appropriate treatment can be started promptly. If you have AMD, regular home use of the Amsler grid (which your eye doctor may provide) can help you monitor changes in your central vision.
The photos at right show a typical Amsler grid. The top photo shows the Amsler grid as seen by those with normal vision. The bottom shows the grid as seen by someone with AMD.
If you notice blurry or decreased central vision, you should call your eye doctor. If you have known AMD and you notice changes in your central vision, you should see your eye doctor promptly.
The Age-Related-Eye Disease Study (AREDS), a ten year study sponsored by the National Eye institute, found that a high dose supplement of antioxidents and zinc significantly decreased the progression and vision loss associated with AMD. A suggested formula would include daily intake of Vitamin C (500mg), Vitamin E (400IU), Beta-carotene (15mg), zinc oxide (2mg) and cupric oxide (2mg). Some patients with AMD, especially present and past smokers, should not be on these vitamins; thus patients really should discuss vitamin supplementation with their medical doctors. Supplemental beta carotene in particular should be avoided by smokers.
There are several types of treatment for wet AMD, all of which are designed to contain the growth of abnormal blood vessels underneath the retina to stabilize the vision. One treatment involves a conventional thermal, or hot, laser, which cauterizes the abnormal blood vessels. Another is photodynamic therapy, which uses a drug called verteporfin that is injected intravenously. The drug is then activated by a special laser which causes the blood vessels to close. Surgical methods of treatment include include macular translocation, which moves the macula away from the abnormal blood vessels onto a new location of healthier tissue. Patients may be candidates for one or another of these treatments depending on several factors, including the type and location of blood vessels.
Areas of current research include anit-angiogenesis medications such as Macugen injected into the eyeball (to stop the growth of blood vessels), forms of laser therapy such as transpupillary thermotherapy and feeder vessel therapy, and surgeries such as submacular surgery and retinal cell transplantation.
There are several types of treatment for wet AMD, all of which are designed to contain the growth of abnormal blood vessels underneath the retina to stabilize the vision. One treatment involves a conventional thermal, or hot, laser, which cauterizes the abnormal blood vessels. Another is photodynamic therapy, which uses a drug called verteporfin that is injected intravenously. The drug is then activated by a special laser which causes the blood vessels to close. Surgical methods of treatment include include macular translocation, which moves the macula away from the abnormal blood vessels onto a new location of healthier tissue. Patients may be candidates for one or another of these treatments depending on several factors, including the type and location of blood vessels.
Areas of current research include anit-angiogenesis medications such as Macugen injected into the eyeball (to stop the growth of blood vessels), forms of laser therapy such as transpupillary thermotherapy and feeder vessel therapy, and surgeries such as submacular surgery and retinal cell transplantation.
Most patients with AMD do not experience vision loss. For those with decreased vision from AMD, the disease usually does not improve over time, though in some cases it can stabilize on its own. Many currently available AMD treatments are designed to preserve the central vision rather than improve it.
Although AMD can significantly challenge one's central vision, it is important for patients with AMD to know that this disease almost always only affects central vision and almost never will cause them to go "completely blind". In fact, in 99% of cases the peripheral, or side, vision remains unaffected, allowing for independent living.
Although AMD can significantly challenge one's central vision, it is important for patients with AMD to know that this disease almost always only affects central vision and almost never will cause them to go "completely blind". In fact, in 99% of cases the peripheral, or side, vision remains unaffected, allowing for independent living.

Above:
Simulated Vision For A Patient With Advanced Dry AMD.
Simulated Vision For A Patient With Advanced Dry AMD.
There are two forms of AMD, a more common dry form and a less common wet form. In the dry form, which affects 90% of AMD patients, aging deposits called drusen become deposited underneath the macula. In the vast majority of patients, these drusen cause no visual changes; however, in some the drusen can cause the macula to thin, resulting in a slow, gradual decrease in central vision. If the drusen cause substantial weakening of important layers in the macula, the wet form of AMD may then develop. Wet AMD develops when abnormal blood vessels start to grow through the layers of the macula that have been weakened by the dry form of AMD. These abnormal blood vessels can cause bleeding, leakage of fluid, and the formation of scar tissue, which in turn can lead to a rapid and severe loss of central vision. Although only 1 in 10 patients with AMD will convert from the dry to the wet form, the wet form accounts for 90% of the vision loss associated with AMD. The chance of a patient with dry AMD converting to the more agressive wet form is approximately 2% each year.

Contact Lenses | Glaucoma | Just For Fun | Eyeglasses | Eye Doctor | Eye Care And Symptoms | Eye Anatomy | Online Eye Tests | Laser Eye Surgery | Laser Eye Surgery Directory: Canada | Laser Eye Surgery Directory: USA | Laser Eye Surgery Reviews | Submit A Review | Contact Us | Privacy Policy | Sitemap
Copyright 2006-2010 Vision Health

